CHARLIE CONNELLY explores the outbreak of the Spanish Flu and its reminder of mankind’s vulnerability.
At 1600 Clifton Road in Atlanta, Georgia, lives a centenarian. To visit, however, one must don full protective clothing and breathing apparatus and pass through rigorous security checks including fingerprint pads and retina scanners. Not that there would be many well-wishers: this particular hundred-year-old is indiscriminately vicious and, according to computer models, capable of killing 30 million people within weeks. There won’t be much in the way of celebration to mark the centenary of H1N1, the Spanish flu virus.
Private Albert Gitchell had had a restless night of hallucinogenic dreams. When the raging sore throat he had developed finally woke him early on the morning of March 11, 1918, he realised his sheets were soaked with sweat and when he tried to swing his legs out from under them pain seared through his nerve endings. The coughing started when he sat up, which only worsened his steam hammer of a headache.
A crippling lethargy made putting on his clothes an ordeal but eventually the mess cook was able to haul himself to the medical facility at Camp Funston, Kansas, where thousands of doughboys trained and waited to be shipped over to Europe to join the war.
When the 28-year-old Chicago native reported to the infirmary he told the staff it was the worst cold he had ever had.
When they took Gitchell’s temperature and the thermometer read 103F the medics realised this was something a little more serious than a cold. Prescribing bedrest they pointed him towards the tent where they housed contagious patients. They couldn’t take any chances: the last thing Funston needed was a fever spreading through the camp. Shortly afterwards an army truck driver named Lee Drake appeared with similar symptoms and he too was packed off to the isolation tent.
Minutes after that Sergeant Adolph Hurby walked in looking, if anything, worse than the first two men. His temperature was a degree higher than Gitchell’s and he too was packed off to isolation.
By lunchtime more than 100 men had presented themselves with the same symptoms; after a week the number had grown to more than 500, before long it was 1,100. Most of the men recovered after three to five days but 48 died. The medical staff were mystified; their best guess was that this clutch of seriously ill patients was down to fallout from a recent dust storm mixing with the ash from burning horse manure at the edge of the camp. They were wrong.

Alfred Gitchell recovered and after the war lived quietly, running a restaurant in South Dakota. But within 18 months of his feverish night a hundred years ago, the H1N1 flu virus of which he was the first recorded sufferer would kill between 50 and 100 million people around the world and infect around 400 million more.
They called it the Spanish flu but it wasn’t a Spanish creation. For one thing, in addition to Camp Funston, later researchers identified possible roots of the virus in Shansi, northern China, at the end of 1917, while at the vast British army holding camp and processing centre at Étaples, 20 miles south of Boulogne, hundreds of soldiers had gone down with flu-like symptoms during the winter of 1916-17.
The Iberian sobriquet became attached because, as a neutral country, the Spanish press wasn’t subject to censorship restrictions and reported openly on the spread of a virus that would infect eight million Spaniards including the king. Borders meant nothing to H1N1 as it incubated enthusiastically in large army camps with a high turnover of men who were subsequently transported in large numbers over long distances, and capitalised on global shipping and rail networks to rampage around the world respecting neither race, class nor nationality.
One in four Americans were infected, 675,000 of them fatally (the US military suffered more fatalities through Spanish flu than it did in First World War combat).
Barely a month after the Camp Funston outbreak the Allied troops on Europe’s Western Front began falling ill until half of them were infected, while across No Man’s Land an estimated 900,000 German troops went down with the virus. In India something close to 14 million people died, six per cent of the population.
In the space of a few weeks the influenza pandemic had reached communities as disparate as Ethiopia and the western tip of Alaska. Walt Disney caught it, as did Kaiser Wilhelm, Ezra Pound, Haile Selassie, Franz Kafka and the British Prime Minister David Lloyd George. Some 400,000 people would die in France, while the 38,000 fatalities in Tonga represented around 20% per cent of the entire population.
In a Britain still coming to terms with the scale of the slaughter in the trenches across the Channel, something approaching a quarter of a million people died as a result of the epidemic. In the spring of 1918 Walter Cook, a 19-year-old stretcher bearer from London home on leave from the front, was stunned by what he saw.
Have your say
Send your letters for publication to The New European by emailing letters@theneweuropean.co.uk and pick up an edition each Thursday for more comment and analysis. Find your nearest stockist here or subscribe to a print or digital edition for just £13. You can also join our readers' Facebook group to keep the discussion and debate going with thousands of fellow pro-Europeans.
‘My aunt who lived in Knightsbridge said she heard I was home and told me her boy was seriously ill in the flu epidemic and could I come and look at him,’ he recalled.
‘I spent the rest of my time nursing this boy but he died the day before I went back. Fourteen years old, he was a lovely lad. I never left him. Mother had a girl from the country, working at the Woolwich Arsenal or something, she died in bed upstairs. A bonnie girl, it was as quick as that. I couldn’t understand it.’
Cook’s level of incomprehension at the speed and virulence of the epidemic was shared in every country on every continent: the only major population centre in the world not to report a single case of Spanish flu was Marajo, an island in the Amazon delta.
In Spain they called it the ‘Naples Soldier’ after a popular song of the time. In West Africa it was Brazilian flu, in Brazil it was German flu. To the Poles it was the Bolshevik disease while in Persia it was the British disease. In some places it was referred to as the ‘three-day disease’, because if it didn’t kill you that’s how long it was before you began to recover.
It was just as deadly whatever you chose to call it – the global mortality rate was the highest in recorded history with the virus proving fatal in 20% of people who caught it. In most flu outbreaks that percentage is nearer 0.1.
There were astonishing reports of how fast the virus acted. From the first symptoms it was sometimes only hours before sufferers displayed evidence of cyanosis, a sickly pale hue that was almost lavender in colour, indicating the patient’s system was starting to break down and death was near.
One night in the US four women friends played bridge until late into the evening and the next morning three of them were dead. There was a report in Chicago of a man who felt well enough to catch the trolleybus to work but who was dead before it had travelled six blocks.
At the end of October, when the epidemic was at its height, the Charlie Chaplin three-reeler Shoulder Arms opened at the Strand Theatre in New York and did good business, prompting the cinema’s managing-director Harold Edel to comment, ‘We think it a most wonderful appreciation of Shoulder Arms that people should veritably take their lives in their hands to come and see it’. A week later Edel was dead from Spanish flu.
He was only 28 years old, which was another strange aspect of the outbreak. Normally epidemics of this kind would prey on the vulnerable: the elderly, the infirm and children, yet Spanish flu seemed to target young, healthy adults.
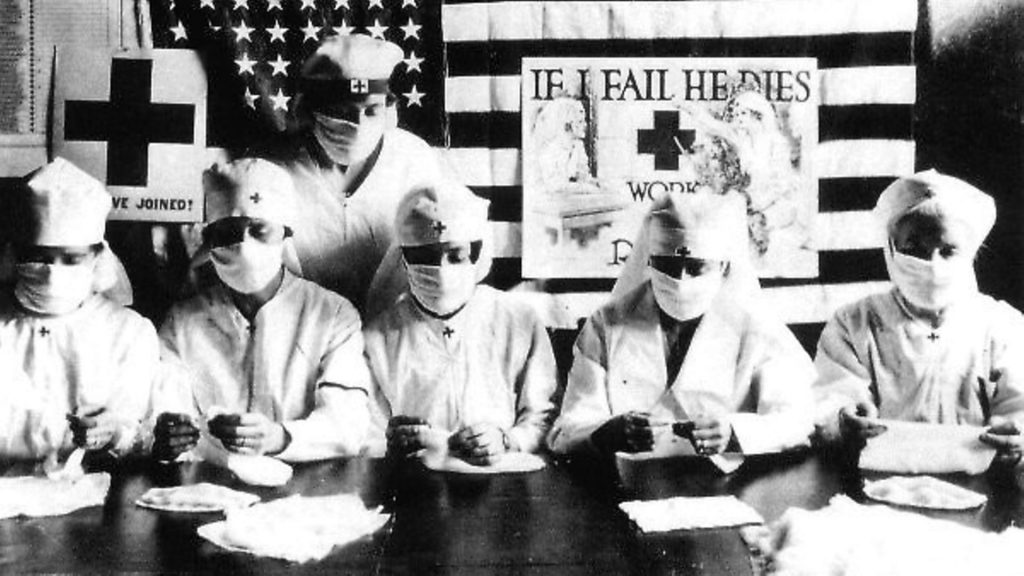
The casualty numbers among the over 65s were relatively minor while so few children were affected that when it was suggested American schools should close until the outbreak passed, the low infection rate among the junior population saw them kept open as valuable centres for disseminating medical advice and information via the children.
The epidemic came in three surges during 1918, the first in March, then September and finally around November. The September outbreak was by far the most virulent strain of all as the virus proved capable of mutating with frightening rapidity. It seemed to break out simultaneously in centres at Brest in France, Freetown in Sierra Leone and Boston, Massachusetts.
Brest was a major disembarkation point for American troops arriving in Europe; some ascribe the Freetown outbreak to infected sailors; while Boston was a major supply port for the war effort.
At Fort Devens, a military camp near Boston, a doctor noted at the end of September, ‘This epidemic started about four weeks ago and has developed so rapidly that the camp is demoralized and all ordinary work is held up till it has passed. All assemblages of soldiers taboo. These men start with what appears to be an ordinary attack of ‘la grippe’, or influenza, and when brought to the hospital they very rapidly develop the most vicious type of pneumonia that has ever been seen.
‘Two hours after admission they have mahogany spots over their cheek bones and a few hours later you can begin to see the cyanosis extending from their ears and spreading all over the face, until it is hard to distinguish the coloured men from the white. It is only a matter of a few hours then until death comes, and it is simply a struggle for air until they suffocate. It is horrible. One can stand it to see one, two or 20 men die, but to see these poor devils dropping like flies sort of gets on your nerves.
‘We have been averaging about 100 deaths per day.’
The final burst of infection came around the time of the Armistice in November, when celebrations brought unwittingly infectious people onto the streets as part of the joyful crowds.
That month a nurse at a casualty clearing station in northern France reported, ‘We moved up to St André after the army went into Lille and almost immediately we started taking in wounded and many who had Spanish influenza as well.
‘The boys were coming in with colds and a headache and they were dead within two or three days. Great big handsome fellows, healthy men, just came in and died.
There was no rejoicing in Lille the night of the Armistice’.
It must have felt like the end of the world. There had never been a global epidemic on this scale before, certainly not since the Black Death at the end of the 14th century, and as it rampaged through a world already traumatised by four years of war on an unprecedented scale it must have seemed at its height as if nothing could stop it.
As an apocalyptic war gave way to an apocalyptic plague, life itself must have seemed under threat. The US army’s Surgeon General Dr Victor Vaughan even speculated whether the virus might spell the end of civilisation altogether.
Instead, as the spring of 1919 headed into summer, the virus seemed to die out almost as quickly as it had spread, probably through a combination of quickly-improvised medical treatments and preventions and a further mutation of the virus strain to a less deadly one.
Yet despite the epidemic killing far more people around the world in a year than the First World War managed in four, the Spanish flu episode soon sank from the historical narrative. It was almost as if, overlapping the horrors of war as it did, the outbreak was too monstrous to comprehend.
Maybe the high proportion of casualties among the armed forces had something to do with the silence that fell over the outbreak: we expected sacrifice from these young men yet we couldn’t keep them safe from disease. Whatever the reason, the virus faded away, the dead were buried and life, which had once seemed so grievously threatened, went on.
For all its prevalence the cause of the Spanish flu virus remained a mystery for decades. Where had it come from? Why was it so lethal, especially to the youngest and healthiest sector of the population? Nobody had an answer and nobody seemed interested in finding one.
In November 1918 the Spanish flu had swept through the remote Inuit communities of western Alaska including the coastal hamlet of Teller Mission, whose population of 80 was reduced over the course of five days to just eight.
A steam crane had to be brought in to help bury the 72 victims in mass graves in the frozen ground.
In 1951, Johan Hultin relocated from his native Sweden to the USA to undertake postgraduate studies in microbiology at the University of Iowa. A chance comment by a professor saw him travel with two colleagues to Teller Mission, now renamed Brevig Mission, in the hope that somewhere in the permafrost there might be preserved a sample of the 1918 virus intact enough to reveal why it was so dangerous.
He met three of the eight survivors of the Teller outbreak and was granted permission to excavate one of the mass graves, donning mask and gloves before hacking through six feet of tundra and permafrost, removing tissue samples from four bodies and sealing them in steel containers inside steel boxes. Back in the Iowa labs Hultin exposed a group of ferrets to the virus but they displayed no traces of illness. Hultin’s research ended there.
In 1995, Jeffery Taubenberger, the head of molecular pathology at the Armed Forces Institute of Pathology, decided to revisit the 1918 outbreak with a view to reconstructing the virus to find out both why it was so lethal and where it might have originated.
He pulled from the institute’s archives slides of tissue samples from 78 soldiers who died during the epidemic, two of which came up positive as having died purely from influenza in September 1918 during the epidemic’s most lethal mutation.
Taubenberger found he was able to reassemble fragments of the virus from the samples but not the complete strain, publishing his findings soon afterwards. By chance those findings were read by Hultin who contacted Taubenberger, offering to go back to Brevig Mission to source more tissue samples. Hultin returned to Alaska in 1997 and gained permission from local Inuit elders to re-open the grave he’d visited nearly 50 years earlier.
While the four corpses he had sampled in 1951 had decomposed he found one flu victim he had missed, an overweight woman in her thirties whose frozen body fat had helped to perfectly preserve her organs.
Hultin removed the woman’s lungs, took samples from other organs and passed them on to Taubenberger who, over the next eight years, was able to fully reconstruct the genetic sequence of the deadly H1N1 virus. When he had finished, laboratory mice he infected with the reconstructed strain died almost instantly.
In 2005, Taubenberger and his colleague Terrence Tumpey, from the US Centre for Disease Control in Atlanta, were able to confirm the virus had originated in birds and been passed on to humans. All three possible origination sites in Kansas, Étaples and China had been situated close to poultry. Mess cook Albert Gitchell had plucked, chopped and cooked some of them.
In addition, Taubenberger was able to explain the prevalence of young and apparently healthy victims: their immune systems were stronger than most and went into overdrive to counter the viral threat. Known as a ‘cytokine storm’, the reaction caused excessive inflammation in the lungs which also filled with fluids, essentially drowning the victim from the inside. After nearly 90 years the Spanish flu had finally given up its secrets.
Immunologists around the world are working as we speak to predict the mutations and make-up of common flu viruses in order to construct the most up-to-date vaccines.
Given the advances in medical science over the last century you would think we were well-equipped now to withstand an outbreak as virulent as H1N1. Yet if the strain did ever escape from its lair at the Jurassic Park of disease in Georgia, given how quickly its symptoms take hold could we guarantee treatment being administered in time? If the predictions are right, it would be too late for 30 million of us.
– This article was first published in March 2018 – a century after the Spanish flu began its deadly assault on the world.