Sir John Bell is the most influential figure in British medicine and a man who strides determinedly between academia, business and politics. He also played a critical role in the development of the Oxford vaccine. He talks to MARK MARDELL about how what unfolded.
Last November, Sir John Bell, a man of many hats and master of keeping them all balanced, uttered three words that echoed around the world: “Yes, yes, yes.”
The slightly nasal Canadian twang of one of the UK’s top medical experts has become a familiar voice during the pandemic, measured and reassuring but never bland. Sir John is anything but bland.
The presenter of the programme on which Sir John was speaking, Sarah Montague of BBC Radio 4’s World At One, flung up her arms in joy at his triple affirmation. Her question was one everyone was asking that week. Did the new vaccines mean life should be returning to normal by the spring? After his trio of yeses, Sir John added: “I’m probably the first guy to say that.” He likes being first, being ahead of the pack. Immediately afterwards, some thought he should have been more cautious. What does he feel now?
“I think I was right. What a story this is, let me tell you, beginning to end! Oh my God, we’re getting close to the end, but I’ve got a good feeling about where we are now. People are going to hold me to it. We’ll get out of the woods.”
What a story indeed.
Sir John is at pains to stress he didn’t discover or develop the vaccine, but what he did as Oxford’s fixer supreme could change the world, raise the university’s prestige to new levels and perhaps eventually boost its bank balance by millions.
He’s the regius – that’s what you are meant to call him, not professor or Sir John – regius professor of medicine at Oxford. Not that he’ll care much what you call him, as long as you listen to what he has to say. It is a royal appointment – a chair in “physic” was first established by Henry VIII in 1546. If it sounds like a fusty, musty relic of a bygone age, it is not seen like that now. Not after Sir John has had the job for 19 years.
He tells me, “I’ve got this funny job in Oxford and people don’t really understand what I do. Regius professor is the senior guy who has no executive responsibility. I don’t run anything. I’ve got a PA and an office, and I just talk to people and help people with strategy and recruit people. I have my fingers on most things.”
One fellow Oxford senior academic who is not a wholehearted admirer feels “just talking to people” gives him outsized influence from “behind the curtain”. He describes Sir John as “a very, very astute political operator, a figure of enormous influence, much greater than his job might suggest. He has an immensely strong personality – and he’s developed a slightly mythical quality – his thumbs down can kill an appointment or an investment.”
Being regius is merely his powerbase, his power flows from being the Nexus. Not a real title, but a good way to think of the way he straddles three worlds and moves effortlessly between them, simultaneously translating ideas and making them flesh. First there are the academic jobs and appointments which flow from them – he was previously Nuffield professor of clinical medicine, he’s been president of the Academy of Medical Sciences, founded the Wellcome Trust Centre for Human Genetics, and he chairs the Oxford Health Alliance and the Global Health Scientific Advisory Board of the Bill & Melinda Gates Foundation.
Then there’s the business world – he’s been non-executive director of Roche for almost two decades, he’s on the board of Gentech, he was on the advisory board of AstraZeneca, and he’s founded three biotech companies. The 68-year-old hasn’t slowed down. Just last month, he joined the advisory board of Hakluyt, a strategic advisory company.
Roping these two worlds together is his mastery of the third sphere, government. David Cameron made him “life science champion” in 2011, and he’s kept the confidence of the changing occupants of Number 10 ever since. He’s now on the vaccine task force and SAGE, he’s chairman of the Office for Strategic Coordination of Health Research, and a board member of Genomics England Limited, the NHS Commissioning Board Genomics Strategy Steering Board, the NHS England Genomic Strategy Board, and chairs the Genomics England Limited Scientific Advisory Board.
Another observer says Sir John is almost unique among scientists in his willingness to put in the “hard yards,” pounding Whitehall corridors, knocking on doors, charming, persuading, cajoling, civil servants and politicians.
One former cabinet minister says, “He’s a very effective Whitehall operator, he can communicate ideas to a lay person without treating you like an idiot, he knows how the world works and he’s interested in practical applications.”
One insider who is wary of the power he wields thinks he could have gone far in politics: “He’s as good as Blair but more brutal.” More brutal?
“Brutal in that he’s willing to take very difficult decisions and face up to the consequences.”
One friend who’s watched him in action in Whitehall suggests in a very British world of nods and winks, where positions are understood and understated, his frankness leaves a mark. He doesn’t leave things half said.
At one meeting, at the end of his tether with a very senior civil servant who wasn’t backing his vision, Sir John made an “astonishing attack” which led to a cabinet minister telling the individual to come to heel and get on board. “He scares civil servants, but they’ve come to rely on him,” this source said.
All of this has made him a central figure in the current crisis.
“I was pretty well trusted by the ministers, then Covid arrived. I was making increasing noises – ‘Come on, we’ve got to get it sorted!’ – so I was the sort of person that ministers and senior civil servants turned to to say, ‘What should we do next?’ So I am in the strange position of trying to orchestrate vaccines and testing and a few other things along the way. My fingerprints are on all of these things.”
One friend of Sir John’s, a senior Oxford academic, says: “He’s obviously someone who can spin a lot plates and switch from one thing to another, he picks things up very fast and makes quick judgements.”
How does anyone have the time to juggle all these things? Sir John chuckles – something he does often throughout our conversation. It’s disarming.
“It’s a good question to ask me now because I feel I’ve bitten off way more than I can chew at the moment. There are some pretty interesting synergies: if you are doing these three things, you can cross reference what’s going on in academia with what’s going on in government and also back to the commercial sector. I’ve been interested in getting universities to think more like biotech companies, to get pharma to think a little bit more like universities, be more grounded in the science and get government to support both.”
*****
Sir John’s story is the story of how Oxford has changed so dramatically that it could beat the rest of the world to a Covid vaccine. It’s a journey which leaves some distinctly queasy.
Bell came from a medical family in Edmonton, Alberta; his mother a pharmacist, his father a doctor, as indeed are his two brothers, one a GP, the other a neurologist. And their personal medical history may be the most important factor in Bell’s career and his determination to turn research into reality.
“My father was pranged in the 1952/53 polio epidemic as many of us were in Western Canada – we were hit in the last wave before they vaccinated us all. The vaccine had actually been invented when it clobbered us. So my father spent the rest of his life in a wheelchair and I spent a year or so in hospital getting my legs straightened out. It was a fairly tough time.”
He was only a baby then, but as he grew up he was aware that 11,000 Canadians had been “pranged” like his father. He worked in the hospital as an orderly, wheeling bodies down to the morgue. Am I guilty of amateur psychology to see a connection in his life’s mission – or is it obvious?
“Yeah it certainly made me…. I came from such a medical environment it certainly was a logical thing to go into because it was so intriguing from so many angles. I keep telling people these pandemics are not as rare as you think – people forget polio. Polio was a terrible, bloody disease.”
His ambition is ferocious. Recently he identified his long term aims as – take a deep breath – developing the human genome project from scratch, spotting killer disease very early, levelling up healthcare in every part of the world, dealing with a global epidemic of mental health and, finally, introducing more artificial intelligence in the NHS.
“I’ve always had ambitions to paint with a broader brush and try to shoot for high goals. I was a kid from the prairies, and when I arrived in Oxford this was an opportunity to get into all that. If you don’t shoot high, you’re never going to get there, and I’ve been really lucky: I’ve been able to keep my head up and look for big outcomes.”
Arriving in Oxford in 1975 as a Rhodes Scholar, he recalled years later a “sleepy, dreary” period when he was forced by the bitter cold to study wrapped up in coat and gloves. This from a Canadian. One senses a complaint not so much against the British weather but against an ancient indifference to the benefits of modernity, even central heating.
He admired the way Oxford’s scientists had made “brilliant, stunning” advances in medicine in a “slightly hopeless, totally disorganised” fashion. He didn’t think he’d stick around for long in what he remembers as the “ramshackle” wards of elderly hospitals and dismal, draughty rooms. But, apart from five years at Stanford, he’s been there ever since. He says it was the scholarship that first opened the doors that allowed him to do what he does – “operate at a high strategic level”.
I suggest even in his youth he radiated impatience. He chuckles again.
“I got the sense the place had become pretty complacent. A long history of excellence encourages people to sit back and say, ‘We’re good because we know we are good.’ It was pretty frustrating and old and musty. Everybody had a gown on and all that stuff, and it wasn’t the way the modern world of bio medicine worked.”
*****
Oxford was, perhaps still is, haunted by the collective memory of how it allowed a huge medical advance to slip through its fingers in the 1940s. Fleming stumbled upon penicillin, but much of the hard work, the pioneering research, was done by a team of scientists at Oxford. They were advised that it would be unethical to patent the treatment. The big money was made in the States and it cost not only Oxford but the country dear.
Sir John can seem like a one-man whirlwind – “force of nature” is a phrase several people use – but he would be the first to stress he didn’t challenge Old Oxford alone. But he was instrumental in dragging the “sleepy” city out of bed and blinking into the sunlight.
For the very look of Oxford has changed. The buildings from the 11th century, the architecture from Gothic Perpendicular to Gothic Revival are still there, of course, wowing students and tourists alike. But there is a bold new font on the palimpsest. The ancient city is now ringed by gleaming silver buildings like a fleet of spacecraft from the future. Some would see that as an apt image – they bring with them the gift of advanced knowledge, but they can feel like an alien invasion nonetheless.
When I last visited Oxford in the early days of the pandemic (last March) it was to the labs where what’s now called “the Oxford vaccine” was being researched and developed by Dr Sarah Gilbert. She gave me a tour and patiently explained the science and her confidence in developing an effective vaccine. But it was the setting that made another point clear. The rows of benches and equipment, behind secure glass partitions, are contained within swooping metal and dizzying wooden constructs, an ode to progress – and generous outside investment.
When Bell arrived back from the States in 1988, he’d seen the future – and it worked, not least, for academics themselves, and their bank balances.
“I’d just come back from Stanford, where every ‘post doc’ in the building had a business plan in his top draw. Most of the faculty had companies. It was an amazing environment. But at that stage in the UK there was no venture capital, no science parks, no scent of a biotech company. It was really bad.”
A graduate student had made a big advance in the study of diabetes but couldn’t get funding. Sir John helped him set up a biotech company that was eventually sold to the States for $3.5bn. There was literally no place for it in Oxford.
“I realised then, I had to do something to change the dynamic. It was my belief you can’t be a world class university without a technology cluster associated with you – that’s been the driver around the Boston and San Francisco hubs – it’s really enabled those universities to succeed and you can’t succeed if you don’t have them.”
Then a stroke of luck.
The Wellcome Trust sold all its shares to Glaxo and created a massive endowment fund. It was a pot of gold for Oxford – and Sir John persuaded them to set up the Wellcome Centre for Human Genetics on a brand new campus; the cornerstone, he says, of his life’s work.
“I trotted off to the Wellcome and told them, ‘I think we can solve the problem of how genetics contributes to the major diseases: cancer, heart disease’… no one was thinking of that in 1991, no one at all. We chipped away, and it was really slow going. Then in 2010 we made a lot of progress – 25 years later. So I set the direction, I try to bite off pretty big challenges and stick with them as far as I can.”
*****
Sir John has been instrumental in making sure the research going on inside these modernistic buildings doesn’t just end up in peer-reviewed journals. Each passing year more and more research scientists have set up small companies, “spin offs” or “spin outs” in the jargon.
There’s a triple aspiration – to turn their research into real products – and to make money, both for the university and for themselves. These aims can chime together, but they can also create disharmony. For those used to the cliché of a world of dusty gowns and elbow patches, it is a shock to discover some professors have become millionaires.
One former Conservative cabinet minister approves – “Seeing Porsches in the university car parks improves morale all round.”
Others are less sanguine. One senior academic says, “I’m not a big fan of spin outs because they pull academics out of the university into companies and they may move away from their research. I do feel that financial drivers may distort the direction of travel. Personal financial benefit can distort the direction of people’s work or hinder it by distorting their mission – they have to become quasi business men, conflicted by financial gain rather than answering the scientific questions.”
One important ally of Sir John’s is adamant this is to miss the point – insisting the real aim isn’t about making money for the university or individuals, “It’s more that we want to get our discoveries into people, and you can’t do that without a commercial partner.”
Sir John is characteristically blunt about the advantages of “spins outs” over research limited by academia.
“Look at the US: the most exciting, interesting, innovative, game-changing science is not happening in universities, but small companies. They’re willing to take very big risks and they don’t have to go through peer review, which is the process that academics use to dumb down any good ideas and flatten them out, so you don’t get anything exciting coming out the back end.”
All that said, Oxford is very clear that money makes the academic world go around and the university is pretty keen on making a profit. The ultimate goal is prestige and a top ranking in those precious global league tables, but hard cash keeps them in the game, competing with those well-endowed American institutions. More than half of the university’s income is from other sources than education and research. That includes the sale of spin outs – worth around £10 million in 2018/19 and the return on investment in such companies, £24 million.
The university says in recent years it has “supported the incorporation of 139 companies based on research and intellectual property developed at the university. The value of the university’s equity share in these spinout companies has continued to grow over the last year to £171.4m.”
Given that many see him as the man behind the push for profit, it is surprising that Sir John thinks Oxford has made a classic mistake – greed.
“Most of the reason that the ecosystem for university tech transfer and small biotech doesn’t work very well in the UK is that universities are trying to skim as much as they can out of the system – 40% of the equity. That doesn’t leave much for anyone else. Too greedy. It’s not about making a huge amount of personal wealth.”
A former minister independently highlights the same problem as the flaw in the whole money-making project: “Oxford takes too much equity.”
A friend of Sir John’s, who is enthusiastic about spin outs in general, adds a note of caution about the attitude of the scientists themselves: “Increasingly, academics are becoming entrepreneurs – but it is a completely different skill set. Look at the Oxford vaccine. The thing that made it possible to move forward rapidly was funding from the Department of Medicine to do some critical experiments. That money came from the university, not a spin out.” That is a rather more pointed comment than it may first appear.
The development of the Oxford vaccine saw Sir John deploy his skills as a fixer to the full, to the irritation of some. It both justifies his vision and highlights some of the awkward conflicts inherent in it. The vaccine was forged not just in the lab but in a clash of wills.
*****
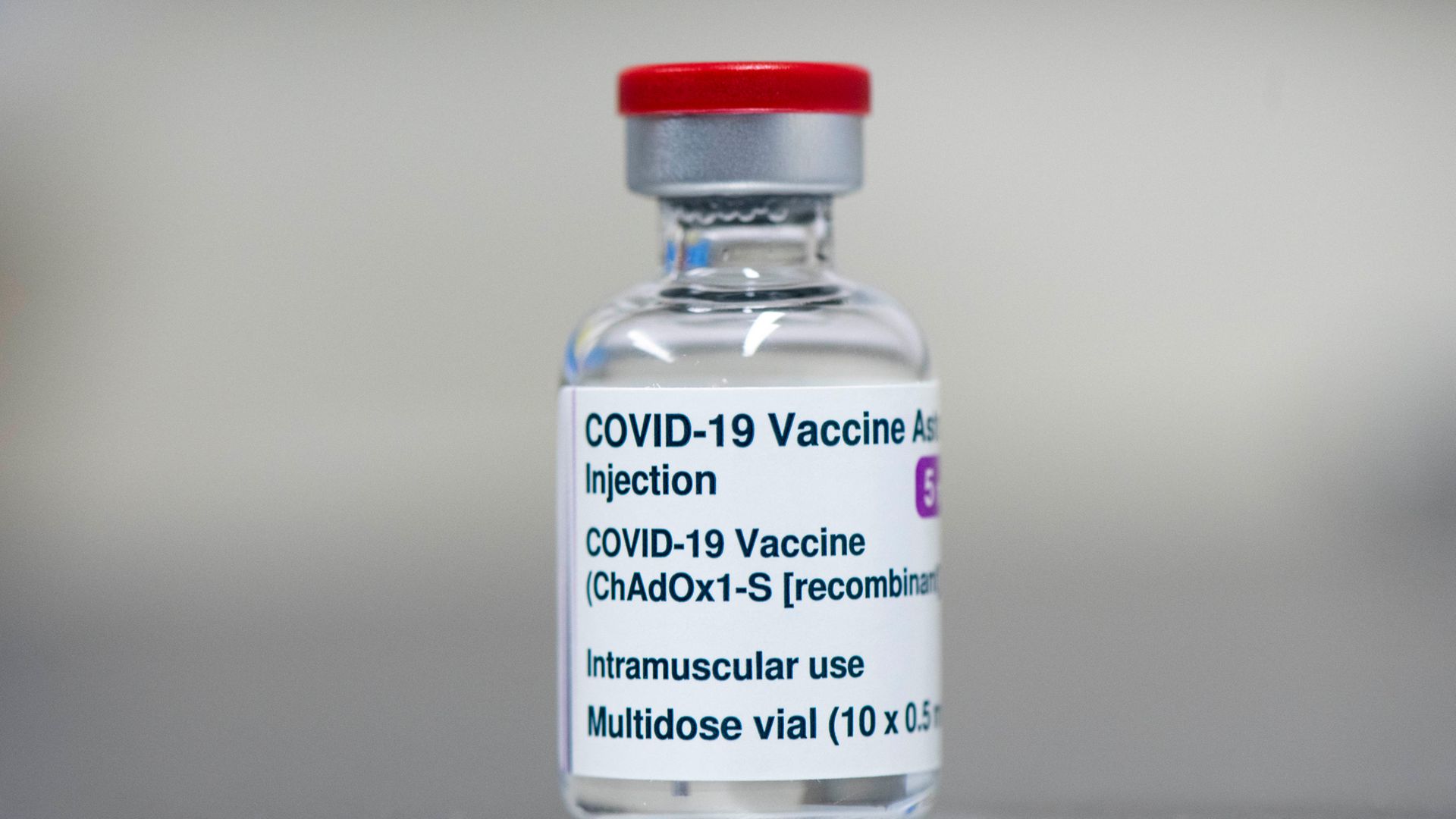
The vaccine was born at the Jenner Institute, developed by Professor Sarah Gilbert. In 2016, she and the institute’s director, Adrian Hill, had founded a spin out company, Vaccitech. At its very heart was the patent for a vaccine based on the virus which causes the common cold in chimps.
This science, based on 20 years research, is what makes the Covid-19 vaccine possible. It is why Sarah Gilbert’s team was so confident it could be produced quickly.
But it also embodies the overlapping, sometimes conflicting, roles inherent in spin outs – at the same time, Sarah Gilbert and Adrian Hill were, and are, both high-powered academic researchers beholden to Oxford University and biotech entrepreneurs with close links to the company they founded.
Early last year, Professor Gilbert had already created the vaccine with considerable help from Vaccitech, meaning both the university and the company felt they had the right to license it. All sides of the conundrum now feel this was complicated and unsatisfactory.
Sir John certainly agrees. He tells me the team at the Jenner Institute are “terrific”, but last February he thought Oxford as a whole risked failure and being blamed “because we screwed up the manufacturing”.
“Remember these are academics – smart people, with a really great focus on emerging viral infections for years – but they don’t look like any vaccine company on the planet because they’re a load of academics in an academic setting doing the best they can, funded by grants.” He adds, “It was rapidly becoming clear we were out of our depth, swimming in pretty deep water, and there were multiple things that worried me.”
Sir John’s central concern was that a four-year-old spin out like Vaccitech wasn’t up to the huge scale of the task ahead. “They had never made a vaccine before, had no way of making it in huge quantities, had no experience with getting regulatory approval or distributing it to the public.”
Those involved say they always knew that they had to have bigger partners but felt that even without them they could make a big impact. By March, the Jenner was already transferring manufacturing technology to China, to India and to many parts of Europe, and looking for more manufacturers. The thinking was that even if the Jenner could not get a big partner, these contract manufacturers would be able to do a lot. Even now, it is these companies who are actually making the stuff.
Another insider suggests there was not only a certain sense of ownership, but that those at the Jenner Institute were simply used to years of work, and repeated failures in the lab, before huge companies were remotely interested in getting involved.
Every conceivable model was discussed, including the university setting up its own company, “Covid Vaccine PLC,” but none went very far.
*****
Sir John was seriously worried. “If you are going to pretend you are going to make a vaccine, you’ve got to pretend you can do all the other things as well.”
Given his experience with so many spin offs, I found it curious when he told the Wall Street Journal that he felt the early days of developing the vaccine were like “Heading into the jungle without a machete”. Why the fear of the undergrowth?
“This was massively different, it needed a big scale, it was a vaccine for the whole world. Starting spin offs is relatively easy. You start with an idea and you have to make about 100 doses for testing and it can take five to eight years. We were way out of our depth here, and if this unravelled, people would be quite justified in being angry for not being sensible.”
Sir John’s “we” is diplomatic – he thought the job was too big for either the university or a small biotech company to handle alone. He knew exactly what he wanted: the involvement of a really big, experienced player. The Nexus pulled out his extensive contacts book.
He says he knew all the heads of R&D and the CEOs of big pharma, so he got out his list and thought, “Who do we talk to?”
His first answer was GlaxoSmithKline. They weren’t interested. Neither were Roche. Then there were talks with huge US companies like Merck.
The academics baulked. They were frustrated, they thought the pharma giants were showing an utter lack of urgency. Not only were they too slow, they thought big pharma’s aim was in direct conflict with what was deep in their own DNA – putting global public health first. By contrast, these big players seemed keen on making a vaccine mainly for the States which would boost their share price.
One of those involved told me, “We were not trying to make a vaccine for rich countries. We were trying to make a vaccine that could be affordable and deployable on an unprecedented scale for the entire world and we wanted a partner that could do that.”
Their insistence had top level support at the university. The vice chancellor, Louise Richardson, added a new condition: not only must the vaccine be available to the whole world, not just the well-off West, she insisted it had to be made without profit while the pandemic raged.
Sir John agreed with these conditions, but says they made negotiations with pharmaceutical companies “a nightmare”.
The writing was on the wall – it was clear these conditions were probably too tough for many potential partners when they could see their rivals hoping to make six billion dollars a year out of their vaccines almost immediately. Oxford were fast running out of viable options.
The academics took matters into their own hands on the prompting of a well-connected friend outside the university.
It was the Jenner Institute’s director, Adrian Hill, who first contacted AstraZeneca. It is a medium-sized British-Swedish company, with a history stretching back to 1913, although its current incarnation is just 20 years old.
The very next day, the company met with a small team of Jenner scientists who faced a slew of detailed questions. But AstraZeneca liked what they heard and, critically, accepted the conditions.
*****
If Sir John was cut out of these initial conversations, he was soon back in the driving seat. His “very good friend”, AstraZeneca’s current CEO, Pascal Soriot rang him to talk about the proposal. Bell knew the company well, too, having been on its scientific advisory board in the past. The conversation convinced him they had found their right partner. The academics are clear that without Sir John’s approval the nascent deal would have died. They were absolutely delighted that he was happy with the plan, but there were more tough conversations before the deal was done.
Vaccitech founders Adrian Hill and Sarah Gilbert might have expected to be at the talks with AstraZeneca themselves, as the scientists at the coalface, but Sir John made it clear that Oxford thought they were “conflicted”. Insiders feel there were those at the university who presumed Professors Gilbert and Hill wielded more influence with the company they founded than they actually did.
Then there were a series of “tricky” conversations with Vaccitech itself. Sir John says, “They said, ‘We’ll do the commercial stuff,’ and I said, ‘Really, how’s that going to work?’ Their last trial had failed, a flu vaccine that had fallen over. This was a relatively small biotech company, this was a global vaccine for the world. No way that was going to work.”
You can be sure Sir John made that argument loud and clear. As the details were ironed out, more problems cropped up, according to Sir John.
“There was a time when they said AstraZeneca should have non-exclusive rights for the vaccine. The danger is: the first guy that manufactures it badly and kills a lot of people then you’re done. The whole thing gets rolled up.”
The CEO of Vaccitech Bill Enright declined to comment on this version of events for this article.
While Sir John’s talks with AstraZeneca were still going on, he managed to wrap up a deal with Vaccitech after more “tricky” talks. In effect, the rights to the vaccine were given back to Oxford University in return for a share of the value. Vaccitech were cut out of future negotiations. A close observer says, while that sounds simple, it wasn’t. They are fairly sure most people wouldn’t have been able to pull it off. Being John Bell, he did.
Although sanguine now, it was a rough time for those at the Jenner Institute. This was the biggest project ever to come their way in terms of global importance and public interest – it could have been purpose-built to highlight their whole mission – and they were no longer sovereign. Sir John Bell and the vice chancellor were calling the shots.
The deal was signed off with AstraZeneca remarkably rapidly. It means Oxford gets no money for six years but then takes 6% eventually. Some estimate that’s worth around £100 million a year.
Everyone involved is said to be very pleased with the outcome, but Sir John’s single-minded approach has clearly left some bruising, if not actual, scars. It is clear from Sir John’s account, things got overheated on more than one occasion.
“Quite a tricky conversation. I had to persuade the academics that the deal with AstraZeneca was as good as they were going to get.
“It was all pretty febrile. A lot of high emotions, people not getting enough sleep, working really hard, and the stakes are high. Back when we were doing this, the stakes were really high because it wasn’t clear we were going to get a way out of this if we didn’t get a vaccine. So it was really hard. We were on the phone 12 hours a day.”
Some of those on the other end of the phone say that, although it was tough at the time, they are “chilled” about it now because they are so pleased with the outcome.
What would those tricky conversations have been like?
A friend says, “He cajoles, he’s not a big threatener.” He admits, “But I’ve never been at the pointy end.”
One high-powered individual who has had a potentially “tricky” conversation with Sir John told me, “He’s absolutely full of charm, but within the space of five minutes he makes it very clear it would take an enormous amount of effort and expenditure of energy to resist his view – he creates an aura of immense influence and makes it clear his network is wider than yours. He’s marmite: some love and admire him; others are wary and fear and envy him.”
Sir John responds: “I’m not sure about fear – people don’t always like the idea that I have strong opinions about things we should do. I don’t always win those arguments, but when I make the argument I am pretty clear about what my thoughts are. If you just roll over on the first lap on the track, you’ll never get anywhere.”
If nothing goes wrong – and there’s a lot of nervousness in Oxford – this vaccine is a perfect showcase for Sir John’s mission, an altruistic money spinner which spotlights the university’s medical and research prowess, burnishing the sense it is still special while making it relevant to those inclined to question elite institutions.
*****
It doesn’t always end up so well. Take the ill-fated foray into private medicine with an American giant.
At the very end of 2018, the American embassy hosted a glittering launch party for a brand-new project – a link between one of the United States’ biggest healthcare companies, Mayo, and a new company, Oxford University Clinics – itself a joint venture between the university and Oxford University Hospitals NHS trust. The idea was to make money out of private patients and plough it back into the NHS and the university, while trying out some cutting-edge medicine at the same time.
Sir John enthusiastically backed it. “All the rationale was great. I was approached by the chief executive of the hospital trust, who’s a real go-getter, a hospital leader, and he was very frustrated Oxford had singularly failed to generate a revenue stream out of private medicine.”
There was another attraction – setting up a clinic to try out some cutting-edge medicine, which Sir John puts with his trademark bluntness. “We were also suffering from the fact the NHS is bulletproof to any significant disruptive innovation. Lots of things we invent… they end up being sold in the US because here in the NHS you can’t even get anyone to answer your phone call. Everyone loves the NHS, but when it comes to innovation they are slow and clunky.”
There was plenty of opposition. Some were furious that Oxford was going to, in their view, undermine the NHS by encouraging private medicine. Others thought the university was guilty of trying to make a profit out of bad practice.
One senior figure who “disagreed quite strongly” with Sir John told me, “I thought it was a bad idea. ‘Well-people screening’ is not validated – It was a rare example of him arguing for something for which there is not good evidence. A number of people made the point at the time that there was no medical benefit. It does matter how you generate money.”
Another academic said at the time that, “If we don’t care how we make money, we might as well open a gin distillery.”
After what he describes as an “active discussion,” Sir John got his way, as you might expect. So he got out his list, went hunting and ended up with Mayo.
The joint venture built a six-floor clinic in Portland Place near Harley Street, designed to give private patients a “health MOT” at £5,000 a pop. It was judged by that go-getting chief executive of the Oxford University Hospitals NHS trust to be an “exciting opportunity”. The Trust’s dry accounts give a glimpse of that excitement, and perhaps a little high-end glamour, listing canapés at the Langham Hotel, a series of dinners, and that embassy do with Mayo clinicians.
The excitement didn’t last.
In July last year, the trust announced a “difficult decision”. They were pulling out. “The clinic in London had performed below plan since opening and turning it around required further investment which the Trust was not prepared to make.”
The money-making scheme was not making any money. Instead, it was losing it.
Oxford University Clinic “concluded that its aims and risk appetite as a public sector entity were no longer closely aligned with the partnership”.
The latest accounts from Oxford University Clinic indicate they suffered a loss of more than £9.5 million after investing £14 million.
Sir John doesn’t seem too dismayed by this failure. “It is a good example of when you shoot high sometimes you fall flat on your face. It fell over. Mayo couldn’t get people to rock up for screening programmes. They’d misjudged the market badly. So it doesn’t take long before you are losing money hand over fist. That was partly my fault. I misjudged how badly the Mayo would misjudge the market. No rain, no rainbows, you’ve got to take a few swings at things.”
A finger in every pie, a fingerprint on every surface, people talk of Sir John’s phenomenal appetite for hard work, his scientific brilliance, his charisma and charm. It is noticeable that detractors say much the same as admirers – they point to his single-mindedness, his determination to win every argument, a forceful determination to get his own way. Sir John probably wouldn’t disagree. He tells me he has thought a lot about how he operates, and how to get what he wants.
“Most people are unwilling to place big bets and say, ‘This might not work, but if it did work, it would be fantastic, so why not have a crack?’. Couple that with a willingness not to give up, never give up. If you think you are right, you must never give up. Sometimes it takes 20 years, sometimes it takes 30 years, but if you think you’ve done the numbers right, then hanging in there and setting ambition really high is really important.”
But that’s not what makes him unique, in many eyes Britain’s most influential scientist, who’s helped turn the dreams of the dreaming spires into hard cash and life-saving product.
It is the rare ability to negotiate the pathways of power in three very different worlds and not become the creature of any one of them. That makes him not just a bridge, for no one walks over Sir John, but the Nexus, the Fixer, the hand behind the curtain.
This article was originally published by Tortoise, a different kind of newsroom committed to a slower, wiser news. To try Tortoise, New European readers can get a 30-day free trial and a special half price offer: just go to www.tortoisemedia.com/friend/trial and enter the code TNE50. You’ll get access to all of Tortoise’s investigations, live editorial meetings, audio articles and daily news briefing emails.