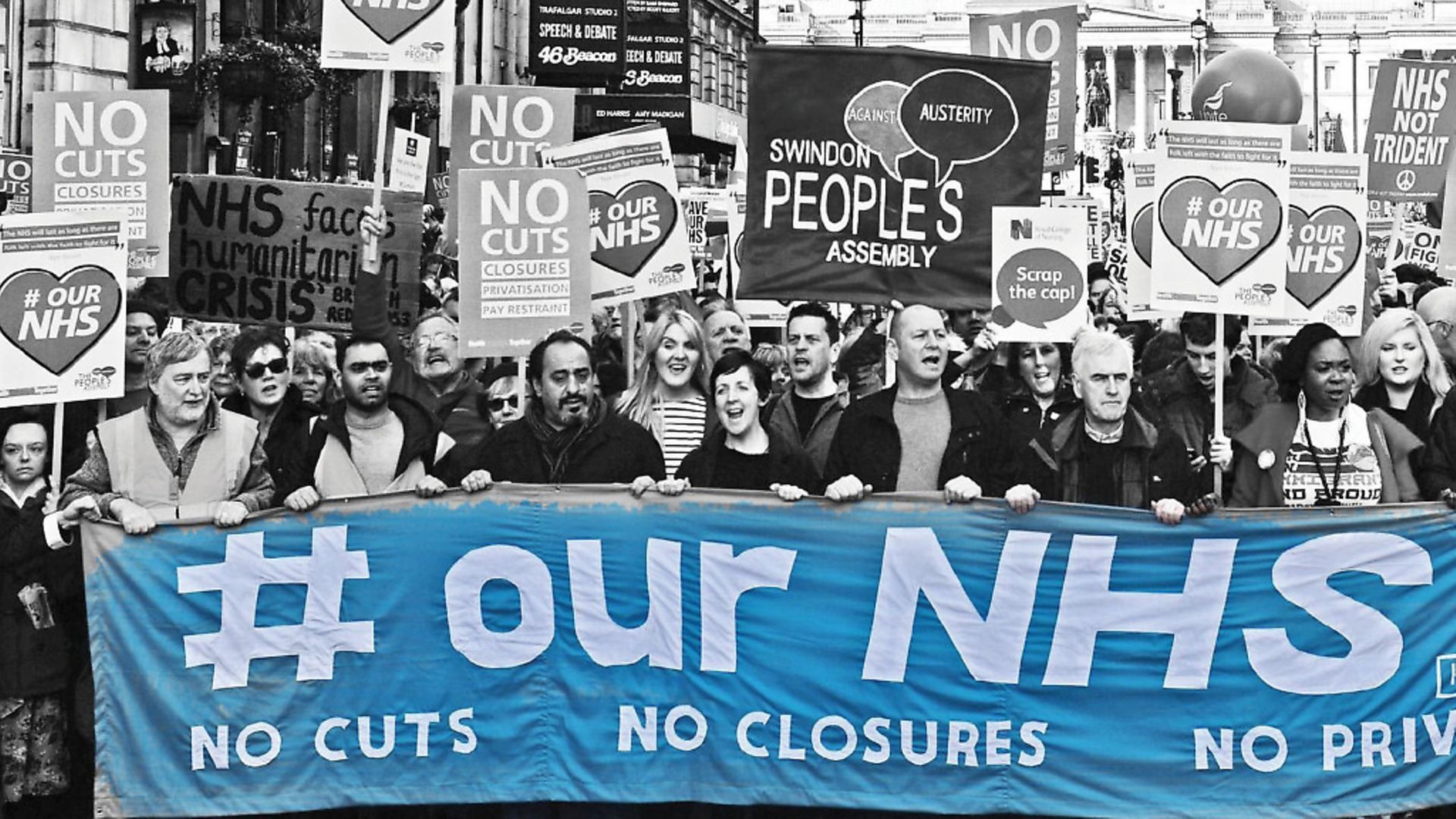
The NHS is Theresa May’s blind spot and it is being sidelined in the Brexit process.
For the last two or three years, the number one concern for most NHS organisations has been their ballooning financial deficits. And with demand for health services and the costs of delivering them still rising at a much faster rate than the government’s funding settlement, sorting out the money is going to remain right at the forefront of people’s minds.
But despite the enormity of the financial challenge – to deliver £22bn of efficiency savings by 2021 – many NHS leaders would now point to workforce concerns as the thing that keep them up at night.
The concerns are numerous and often articulated differently, but essentially boil down to the ability of the NHS to recruit and retain enough staff in order to meet the rising levels of demand.
It worth making clear here that plenty of people still want to work as doctors and nurses, and the numbers have risen substantially over the last few years. The issue is that the numbers are not increasing at the rate required to meet the demand.
There is a lack of reliable data on workforce vacancies within the NHS, but various reports suggest vacancy rates of between 5 and 10% for doctors and nurses (so up to 40,000 posts), which compares to figures of 2 to 3% across the whole economy.
This matters primarily because of patient safety – research has consistently shown that the number of nurses caring for patients is linked to the quality of care. But it also comes back to the money, because the fewer posts that are filled by permanent staff, the more hospitals have to rely on agency nurses or locum doctors who demand a premium rate. And the more the demand for staff goes up, the higher these rates get.
So it’s crucial for the NHS to recruit and keep the permanent staff it needs to ensure the ward rotas are safe and cost effective. This is why the junior doctors pay dispute and strike action in 2016 was so worrying, because it revealed the general sense of unhappiness held by many medics at the start of their career, who the NHS will depend heavily on in the future.
There is a similar sense of crisis among GPs, who will be critical to new models of out-of-hospital care that need to be deployed, while nurses have also started talking about the possibility of industrial action in recent weeks. Pay restraint is obviously prominent in the list of grievances – NHS staff have had their pay increases capped at 1% for the last four years, and had a two-year pay freeze before that.
According to the Health Foundation think-tank, over the course of this decade most staff will have seen their real terms income fall by around 12%, due to the impact of inflation. But probably of greater importance is the increasing pressure on staff, due to that rising demand, leading to greater stress levels and risk of burnout.
So there’s a vicious cycle that plays out here, where the increasing pressures results in more vacant posts, which then ramps up the pressure on the staff who choose to stick it out. Meanwhile, agency work continues to look more attractive for many doctors and nurses – as it offers greater flexibility and a higher rate of pay.
One way that almost all NHS hospitals have sought to fill their rota gaps in recent years has been to use freedom of movement regulations to launch big recruitment drives in other EU countries.
The number of EU nationals in the health service now stands at more than 60,000 (about 5%), which is almost double the figure from five years ago. The number of EU nationals living in the UK increased by 40% over the same five year period, which suggests that EU staff have been propping up the NHS to a much greater extent than additional EU migrants have been putting extra strain on services.
NHS trusts in London have the highest proportion of EU nationals, of around 11% of clinical staff, followed by the rest of the south east with between 6 and 8%. The proportion in the north, midlands and south west ranges between 2 and 5%.
This is why the vast majority of NHS leaders in London and the south east are terrified about the implications of Brexit, and the influence it could have on those who have already moved here, or those who could potentially be recruited in future.
Leaked workforce modelling by the Department of Health recently showed a hypothetical worst case scenario in which the supply of nurses reduces drops out a cliff due to new restrictions on EU immigration, while demand continues to soar.
It is of course too early to start drawing conclusions on the impact on Brexit, but a recent report by House of Commons health committee has noted some extremely worrying early evidence of clinical staff from the EU starting to leave the health service.
Last year, EU staff made up 6.6% of all staff choosing to leave the NHS, up from 5.7% in 2015. The increase was even steeper when nurses were separated out, up from 7.5 to 10%.
Meanwhile, the number of EU nationals joining the nursing register for the first time dipped dramatically in final quarter of 2016, to a monthly average of 204, compared to 820 during the same period in 2015. Much of this drop off could have been due to new English language tests being applied to EU recruits from January 2016, but Brexit may also have been a factor.
One anecdote I heard recently was about a trust holding a recruitment fair in Portugal, which would normally have attracted dozens of young nurses. Only four turned up. So far at least, the situation for doctors does not look so concerning, although NHS trusts are having to do an enormous amount of work to reassure them that their right to stay will be secured.
Many are advising their staff to avoid the complex process of applying for permanent residency, due to the requirement for a non-economically active spouse to hold comprehensive sickness insurance, even if they have lived here for many years.
NHS leaders are desperate for all this uncertainty to be cleared up, and for the government to make a clear commitment on the status of EU workers already here, as well as those which hospitals will rely on in the future. However, it’s not clear that the NHS is being properly considered when it comes to the Brexit negotiations, and the approach being taken by the government.
Health secretary Jeremy Hunt is not a member of the cabinet committee for European Union Exit and Trade, while responsibility for Brexit preparations within the Department of Health has been tasked to just 25 staff who must also continue with their existing commitments.
The department has seen its workforce shredded by 26% since 2010, so there are major concerns about its capacity to assess and influence the potential outcomes, and ensure the NHS is protected from any new limits on immigration. And this plays into a wider concern about Theresa May, and the deprioritisation of the health service in general.
While David Cameron famously summed up his priorities in three letters, N-H-S, the feeling is that May does not understand or have sympathy for its current struggles. She and the chancellor appear to believe their predecessors were too generous to the service, especially in comparison to other departments, and they could well be determined to continue starving it of the funding increases it needs to meet the rising demand.
Although the policy proposals made at the weekend by Hunt, to reform mental health laws, have brought welcome attention to a long-neglected sector of the NHS, there was no new funding announced. So while you might expect a general election to squeeze out helpful spending commitments from the competing parties, the apparent inevitability of the result this time around will allow the Conservatives to be more miserly.
One potential positive of an increased Tory majority though, would be a prime minister less vulnerable to rebellions by her right wing over the Brexit negotiations and the continuing presence of EU staff. In theory, this could provide greater flexibility in terms of their right to remain. If May was that way minded that is. Although the government’s policy is to become ‘self-sufficient’ in its supply of clinical staff, Health Education England has admitted this will not happen quickly. So recruitment and retention of EU staff will continue to be essential to the NHS for another decade at least. Even if the NHS can eventually becomes self-sufficient in terms of its staffing, it will still rely on, and benefit from, the skills and experience of overseas clinicians who wish to build their careers here.
It is in the interests of patients for the NHS to continue recruiting the brightest and best from the EU and beyond, so international recruitment should be made as straightforward as possible.
Lawrence Dunhill is a senior correspondent at the Health Service Journal; follow him @lawrencedunhill