“But now I’ve read the guideline I can’t ignore it!” the trainee implored.
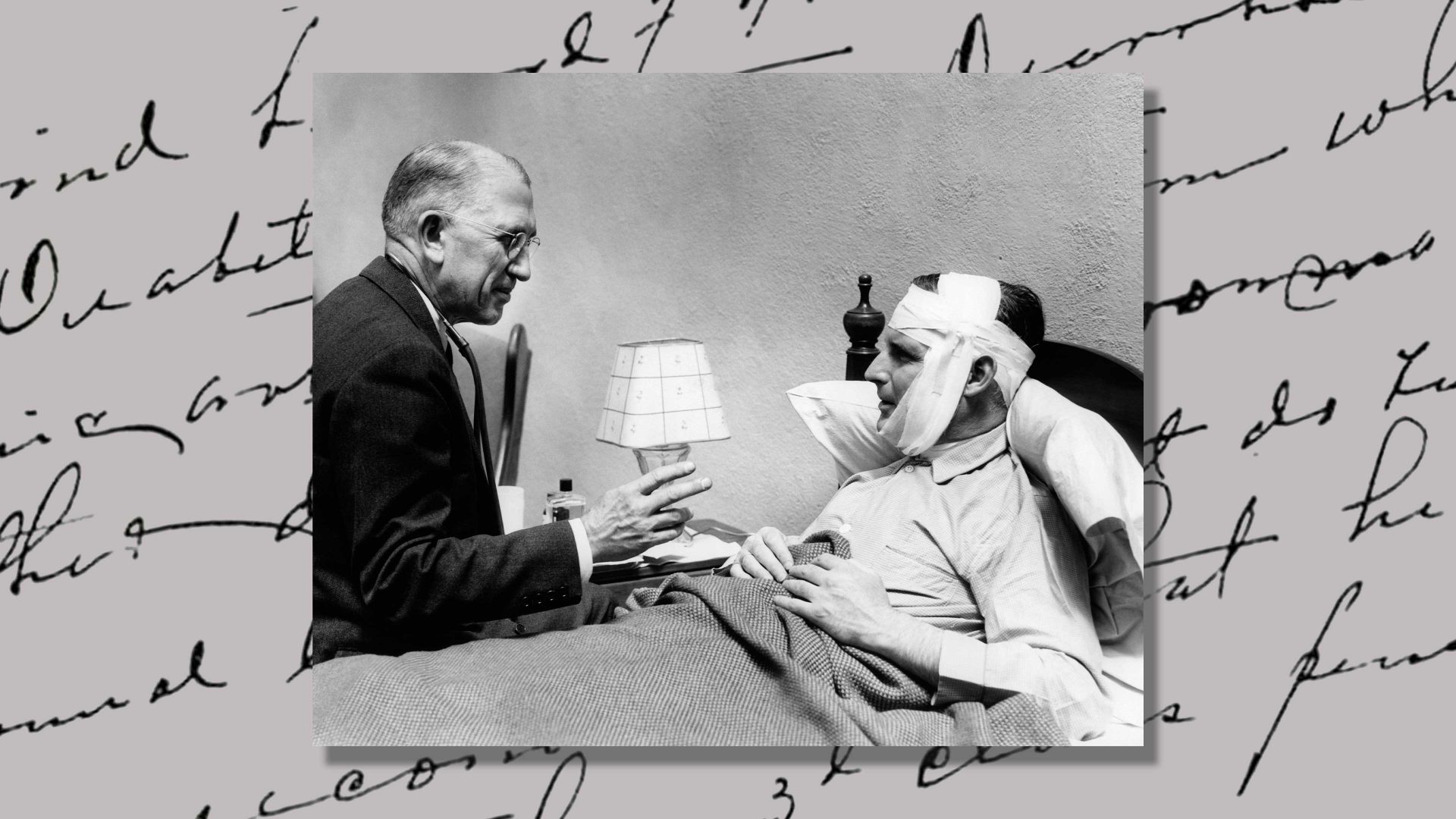
We were discussing one of the cases she had seen that morning – a young man in his early 30s who had wanted to discuss his erectile dysfunction. I tried to imagine how it must have felt for him, nervous and embarrassed, faced with this earnest young female trainee. For all her superficial professionalism, I couldn’t help but admire his courage.
Quite appropriately she had read the clinical guideline, organised some basic blood tests and was now keen to organise the prostate examination it advised.
“Do you have any reason to think he might have trouble with his prostate?” I asked. “Does he have any symptoms? Any prostate problems in his family?”
“No,” she said, a bit uncertainly, “no I don’t think so. I didn’t actually ask – the guideline just says we should do a rectal examination to check his prostate.”
“OK,” I replied. “Well, can you tell me a bit more about him? What about his work? Life at home? Does he have a partner – why has he come about this now?”
“Oh,” she said, again a bit hesitantly, “well I know he works in IT and he said they’re merging with another company so he’s been working away from home a lot. Ummm… and he has a partner. I think they’re married.” She paused again, trying to remember, “and he said something about trying to start a family – but he didn’t really want to talk about it, so I didn’t ask.”
She smiled, trying to be helpful, “I’ve booked him in with me for an examination next week,” she said.
The fear of the guideline has come to dominate much of modern medicine. Although based on evidence and helpful in many ways, the guideline cannot see the patient in front of you. It cannot ask them what they think or wish to do; it cannot tell you what is right or wrong for them – as a person.
The guideline can’t sense the stress of an overworked, exhausted young man facing the expectation and anxiety of a potential family – or the sense of failure and guilt if he can’t have one. It can’t feel the embarrassment and shame of airing the most intimate of failures in public – especially if the audience is a young, attractive doctor. It can’t know that subjecting him to the further humiliation of a physical examination is likely to be both unhelpful and harmful. It can’t know that deep down, he desperately just wants to discuss his fears about the future.
But how can we “ignore the guidelines” to see the patient before us?
All too often our healthcare system values the process above respect and care for the patient. It is why a clinical pharmacist will “persuade” 87-year-old Stan to start a statin, even if he doesn’t want to. It is why, when Joan is admitted to hospital, all the paperwork is successfully completed – the risk assessments and feeding charts; the checklists and logs – but nobody cleans the dried blood from her nostril where it has been irritated by a feeding tube. It is why nobody removes the half-eaten, browning banana and old teabags from her tray, and why she doesn’t know the name of her doctor, or that of the nurse looking after her. It is why she hasn’t seen the same nurse twice.
Nobody knows that she used to be a feisty music teacher, who selected her cottage when she moved closer to her son because it could house her grand piano. Nobody knows that her favourite composers are Chopin and Liszt or that she has two cats and a loving family a few doors away. Nobody knows that all she wants to do is go home to them – nobody has asked.
All the “medicine” in the world; all the evidence; all the guidelines can’t replace the importance of seeing the patient before us and hearing the stories they share. Despite the stresses and pressures, if we cannot find the courage to put the patient ahead of the guidelines and value each individual, our healthcare system may give more harm than care.